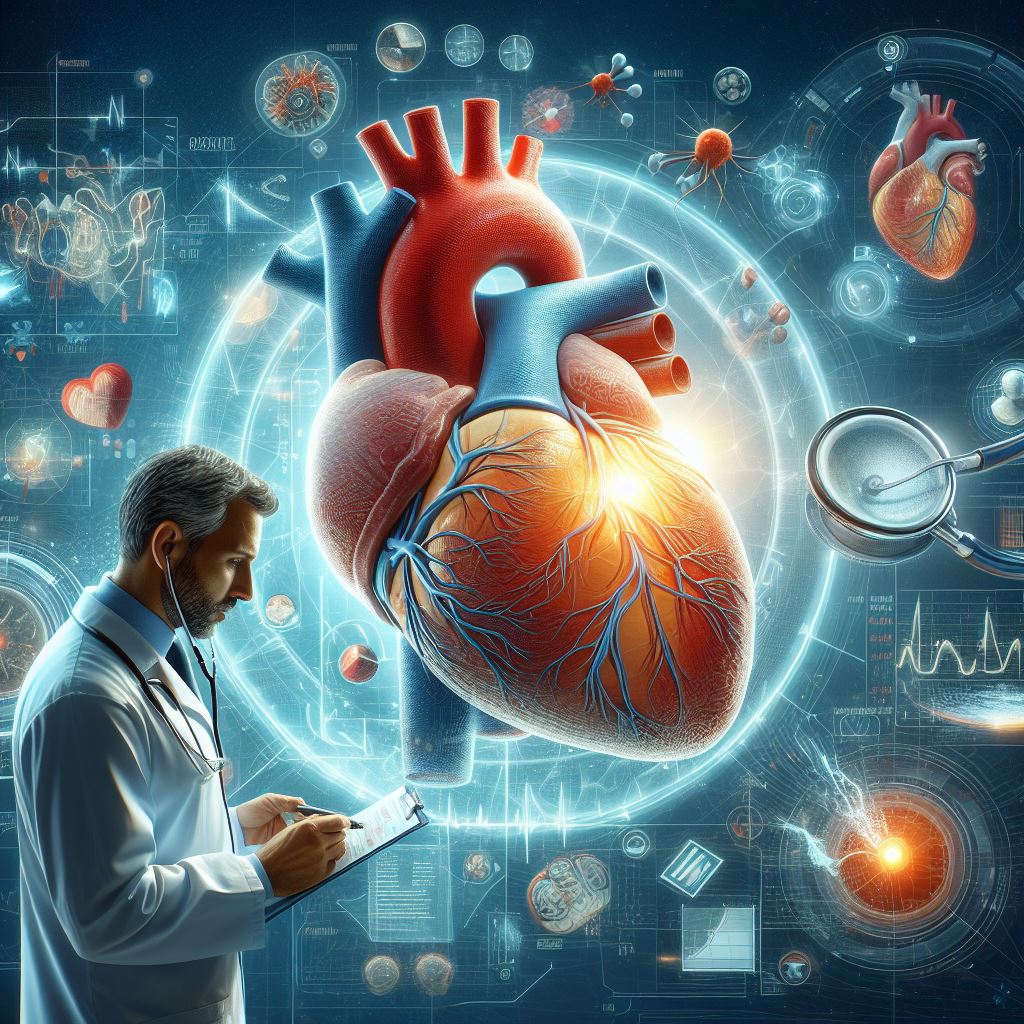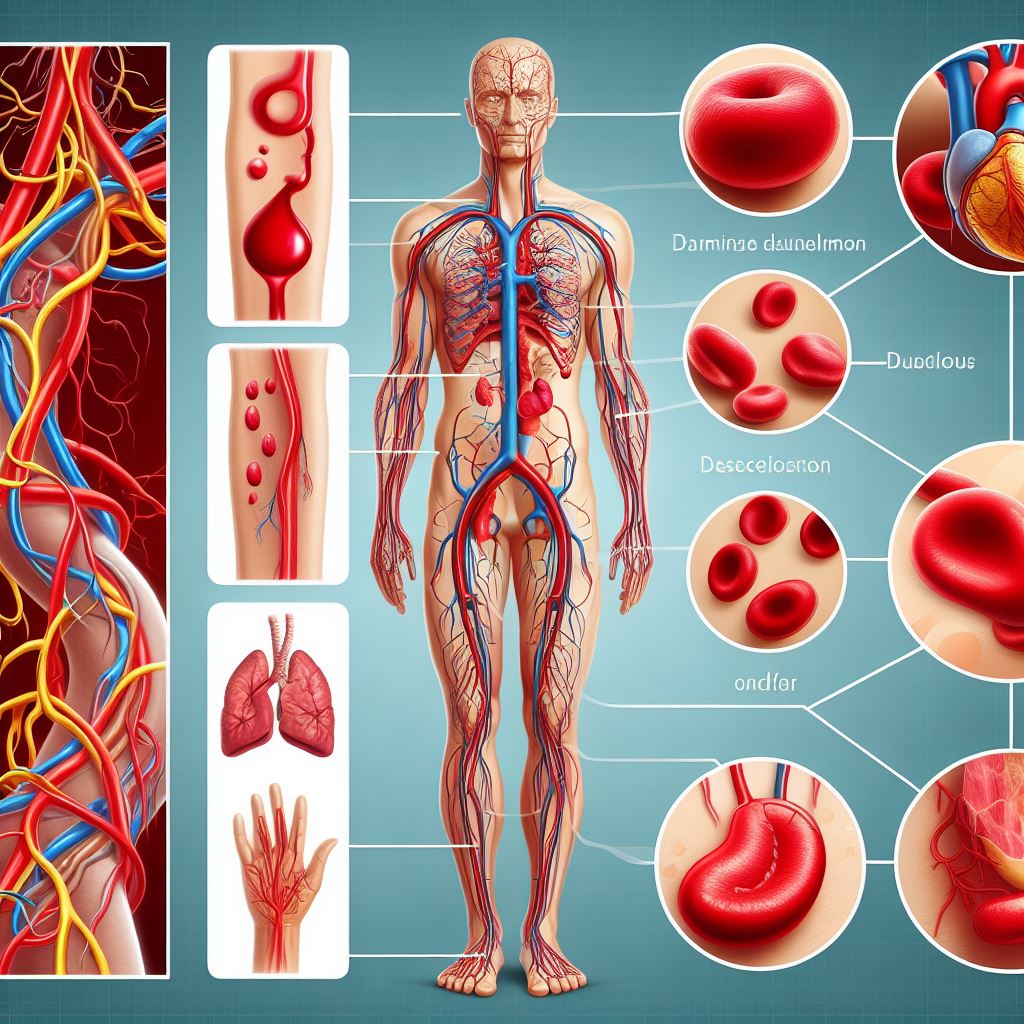
Blood Clots
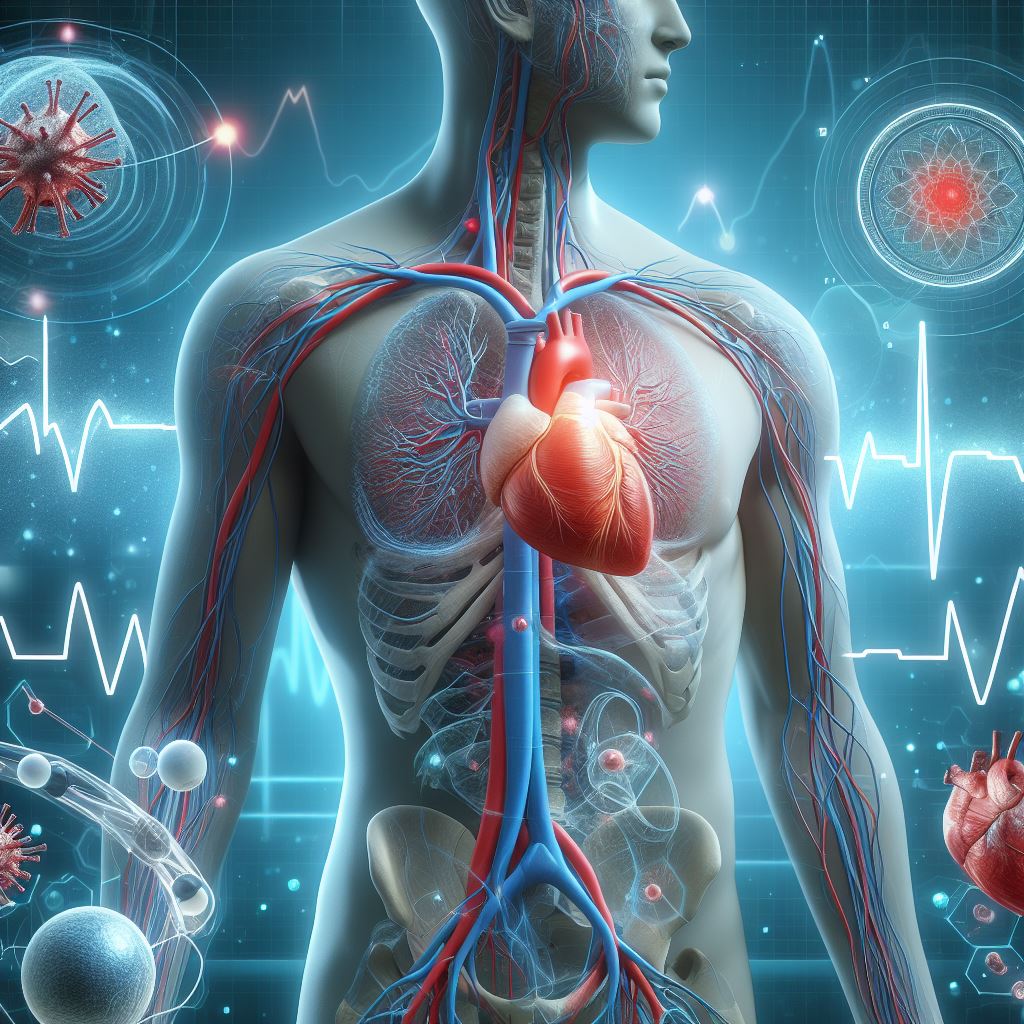
Understanding
blood clots is pivotal for maintaining a healthy heart, and our mission is to
empower you with the knowledge needed to navigate this aspect of cardiovascular
well-being. As we embark on this exploration together, envision a journey that
transcends medical jargon, offering clarity and insights that resonate with
your own journey toward optimal heart health.
Blood
clots, or thrombosis, may sound ominous, but they are a natural component of
the body's defense mechanisms. However, when these clots deviate from their
intended function, they can become a source of concern. This blog post aims to
demystify the topic, starting with the basics – what blood clots are and how
they can impact your cardiovascular system.
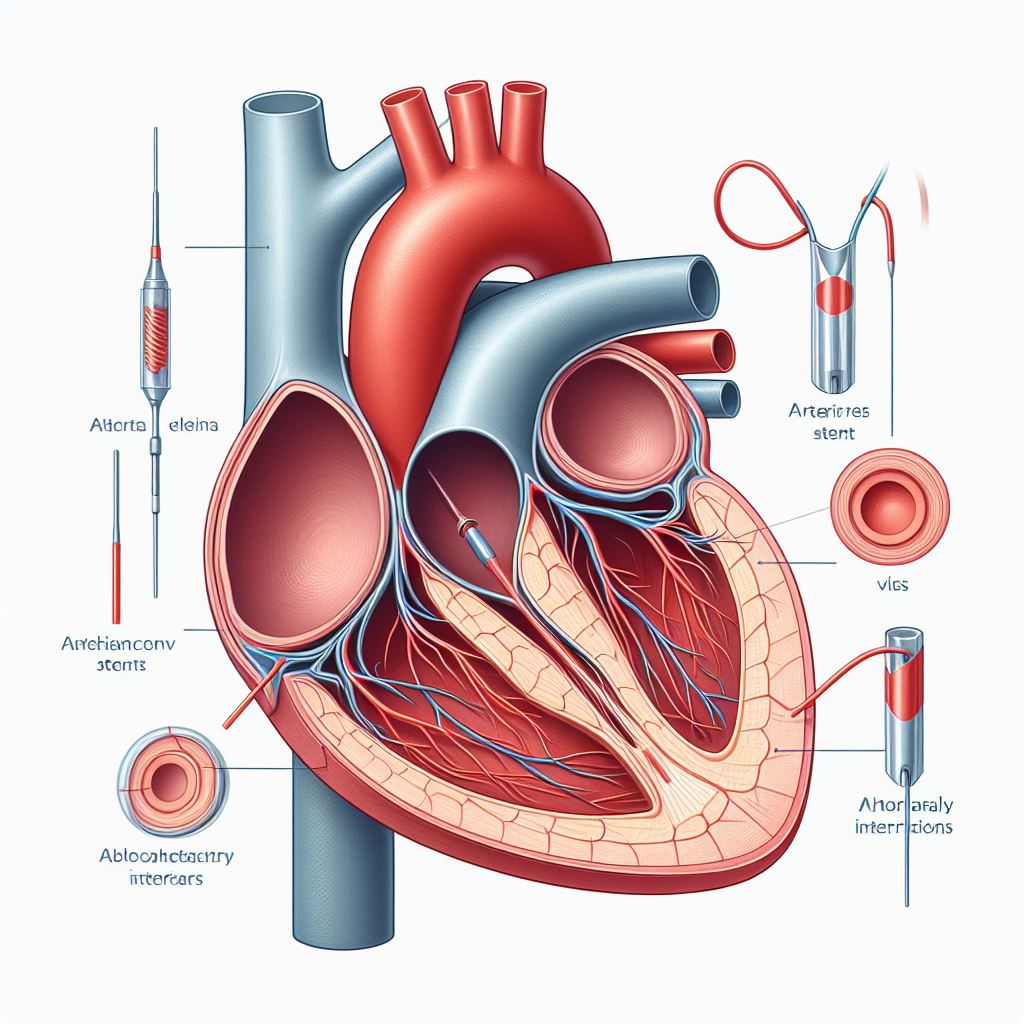
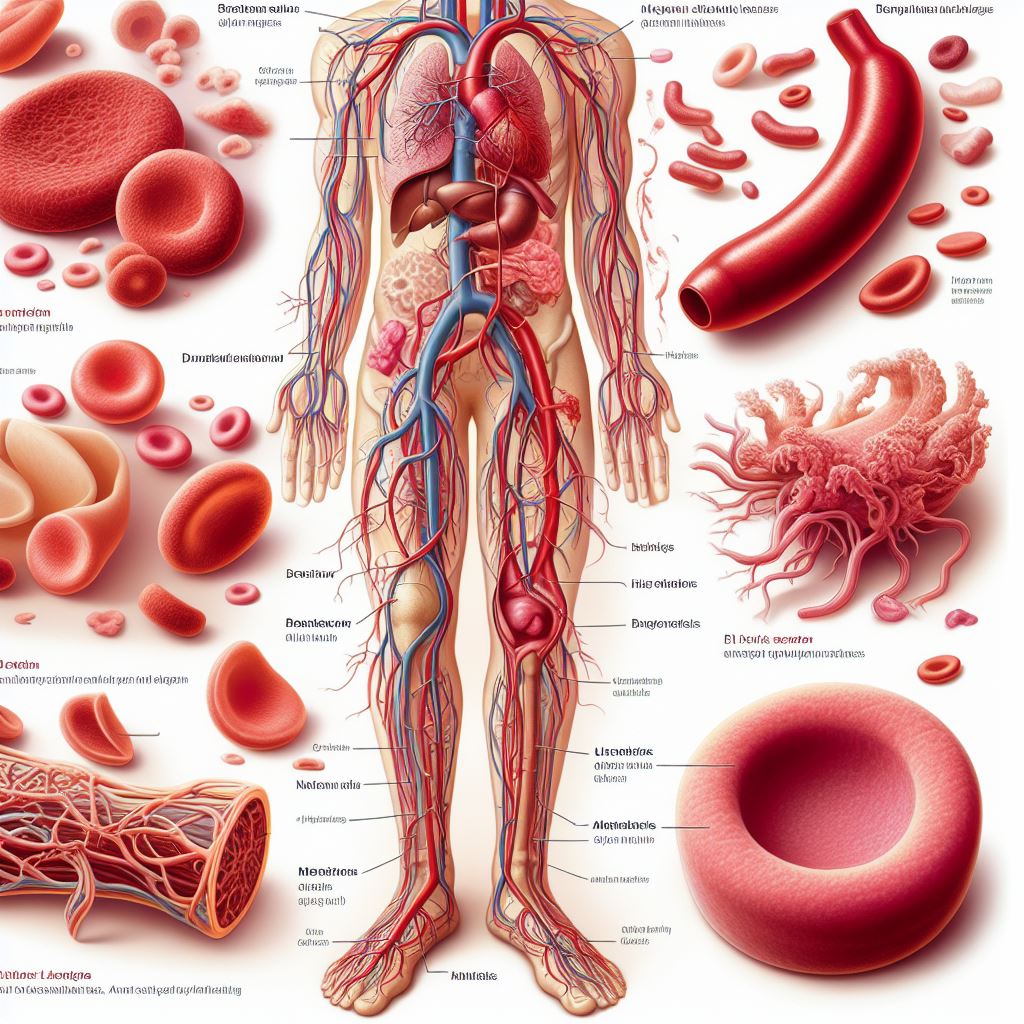
What Are Blood Clots?
Blood
clots, medically referred to as thrombosis, are intricate components of the
body's natural defense mechanism against excessive bleeding. They play a
pivotal role in maintaining the delicate balance between preventing hemorrhage
and promoting healing. Essentially, blood clotting is a complex physiological
process designed to seal wounds and prevent life-threatening blood loss.
However, when this intricate system encounters disruptions, it can lead to the formation
of abnormal blood clots, posing significant health risks, particularly in the
cardiovascular system.
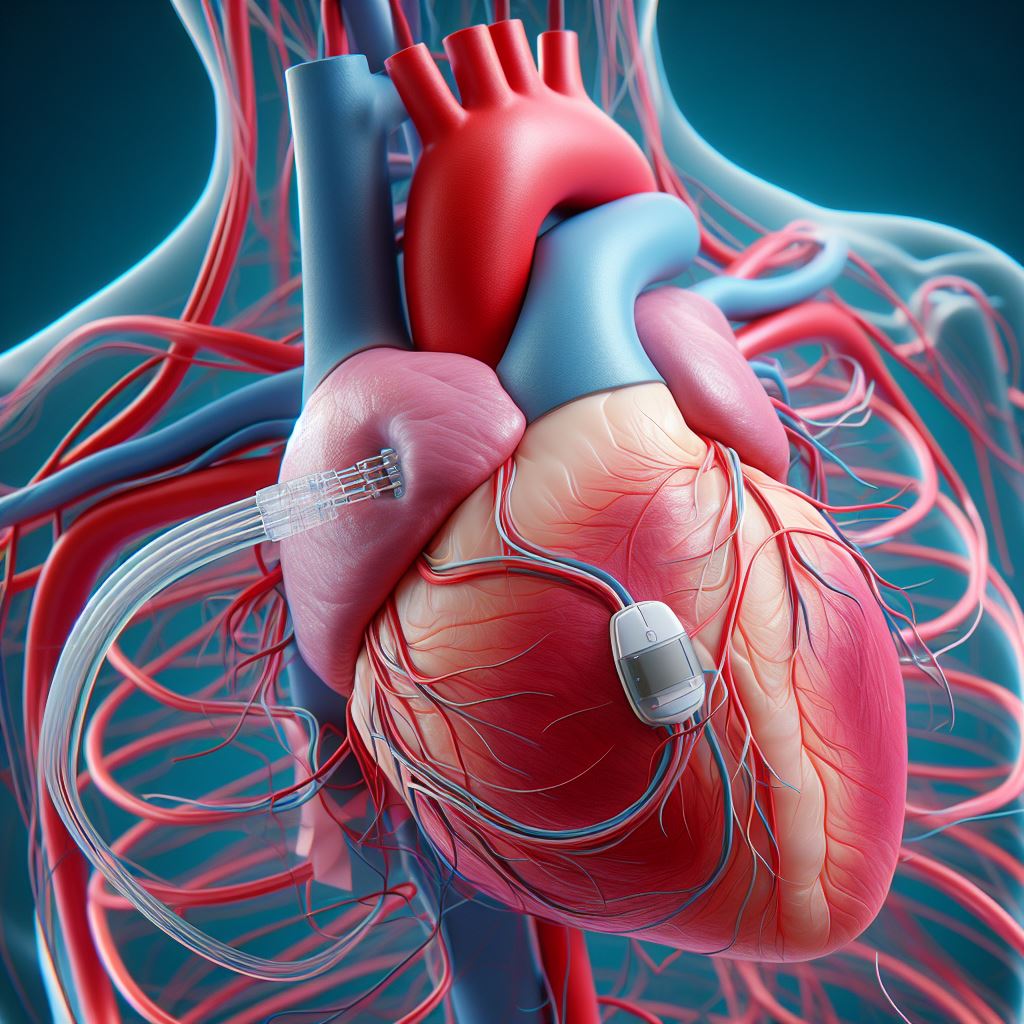
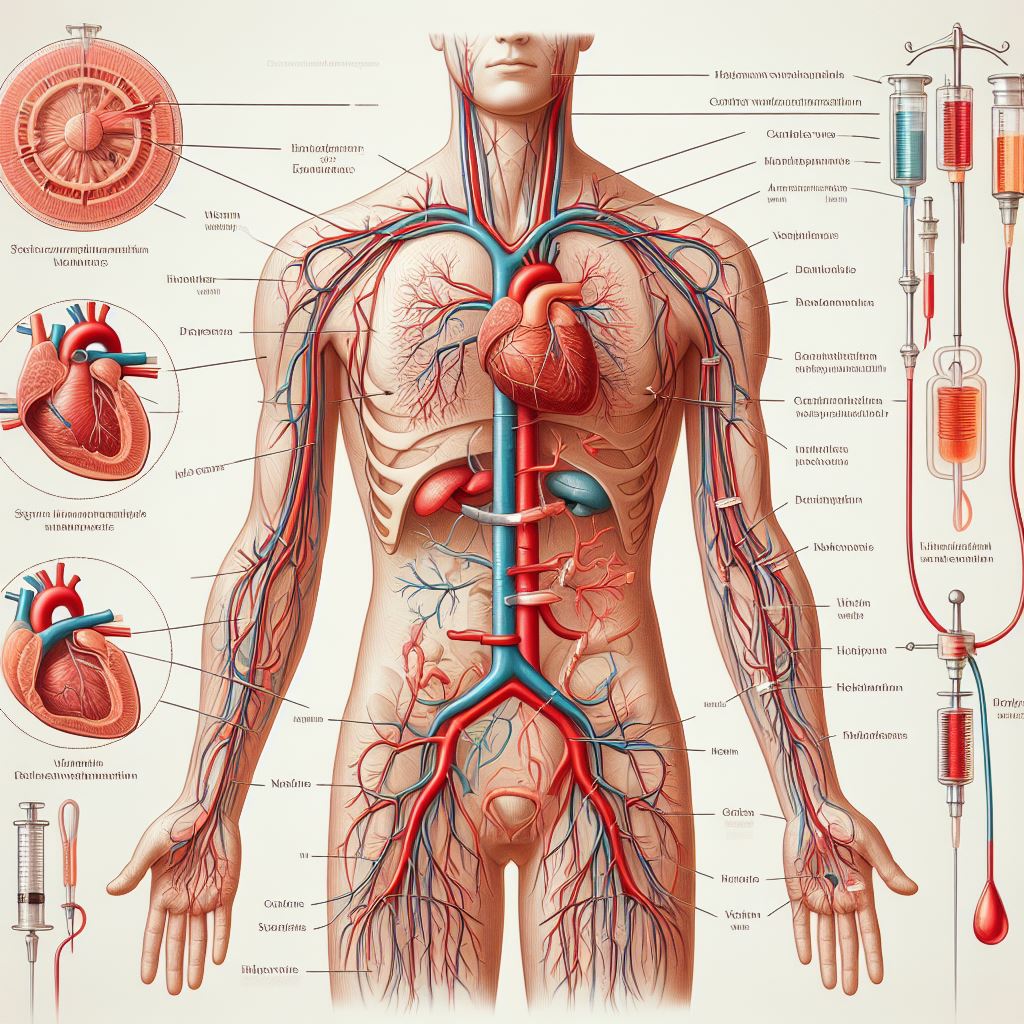
At
its core, a blood clot is a gelatinous mass composed of platelets and fibrin,
two key elements in the blood coagulation process. Platelets, small cell
fragments, initiate clot formation by adhering to the site of injury and
releasing chemical signals that attract more platelets to the scene.
Concurrently, the protein fibrin weaves a mesh-like structure, consolidating
the platelets into a cohesive clot. This intricate dance is finely regulated
under normal circumstances, ensuring that clots form only when necessary.
However,
when the delicate balance is disrupted, abnormal blood clots can arise. There
are two primary types of blood clots: arterial and venous. Arterial clots
typically form in the arteries, impeding blood flow to organs and tissues. On
the other hand, venous clots, such as deep vein thrombosis (DVT), manifest in
veins and pose risks of traveling to vital organs, particularly the lungs,
causing potentially life-threatening complications.
Understanding
the circumstances under which abnormal blood clots may form is crucial. Various
factors contribute to this phenomenon, including genetic predispositions,
prolonged immobility, surgery, trauma, and certain medical conditions.
Individuals with a history of cardiovascular diseases, obesity, or those who
smoke are also at an elevated risk.
The
consequences of blood clot formation can be profound. In the veins, clots can
lead to conditions like DVT, causing pain, swelling, and potentially
progressing to more severe complications. In the arteries, clots may trigger
heart attacks or strokes by obstructing blood flow to critical organs.
As
we navigate the multifaceted landscape of blood clots, it becomes evident that
while they are an integral part of our physiological defense mechanism, their
abnormal formation can have far-reaching implications. In subsequent
discussions, we will delve into the symptoms, diagnosis, treatment, and
prevention strategies associated with blood clots, offering a comprehensive
understanding that empowers individuals to actively engage in their
cardiovascular health journey.
Symptoms of Blood Clots
·
Recognizing the symptoms
of blood clots is paramount for timely intervention and prevention of
potentially severe complications. As we embark on this exploration of
cardiovascular health, let's delve into the nuanced manifestations that may
signal the presence of blood clots in the body.
·
Swelling and Pain:
One of the hallmark symptoms associated with blood clots is localized swelling
and pain. Clots can impede normal blood flow, leading to an accumulation of
blood in specific areas. This, in turn, results in swelling and discomfort,
particularly in the extremities such as the legs or arms. Individuals may
notice a sense of heaviness or tightness in the affected limb.
·
Changes in Skin Color
and Temperature: Blood clots can alter
the appearance and temperature of the skin overlying the affected area. The
skin may exhibit a reddish or bluish tint, indicative of compromised blood
circulation. Additionally, the skin might feel warmer than the surrounding
areas, emphasizing the impact of the clot on normal blood flow and tissue
perfusion.
·
Tenderness to the Touch:
A clot-affected area often becomes tender to the touch. This tenderness is a
result of the inflammatory response triggered by the clot, as well as the
pressure exerted on surrounding tissues due to impaired blood circulation.
Recognizing tenderness is crucial, as it can be an early indicator prompting
individuals to seek medical attention.
·
Shortness of Breath and
Chest Pain: In cases where blood clots migrate to the
lungs, a condition known as pulmonary embolism, symptoms can escalate to more
serious manifestations. Shortness of breath, chest pain, and a rapid heart rate
may ensue. These signs necessitate immediate medical attention, as pulmonary
embolisms can be life-threatening if left untreated.
·
Unexplained Cough or
Hemoptysis: Blood clots in the lungs may also manifest
as an unexplained cough, sometimes accompanied by the presence of blood in the
sputum, a condition known as hemoptysis. This respiratory distress signals a
potential blockage in the pulmonary arteries, requiring urgent medical
assessment.
It
is crucial to note that while these symptoms provide valuable clues, the
presentation of blood clots can vary widely. Some individuals may experience
subtle signs, while others may confront more pronounced symptoms. Additionally,
certain medical conditions and risk factors can predispose individuals to blood
clot formation, further emphasizing the importance of vigilance and proactive
healthcare.
As
we journey through the intricacies of blood clots, understanding these symptoms
becomes a powerful tool in promoting cardiovascular health. In subsequent
discussions, we will explore the diagnostic techniques employed by
cardiologists to confirm the presence of blood clots and outline tailored
treatment approaches for optimal patient outcomes.
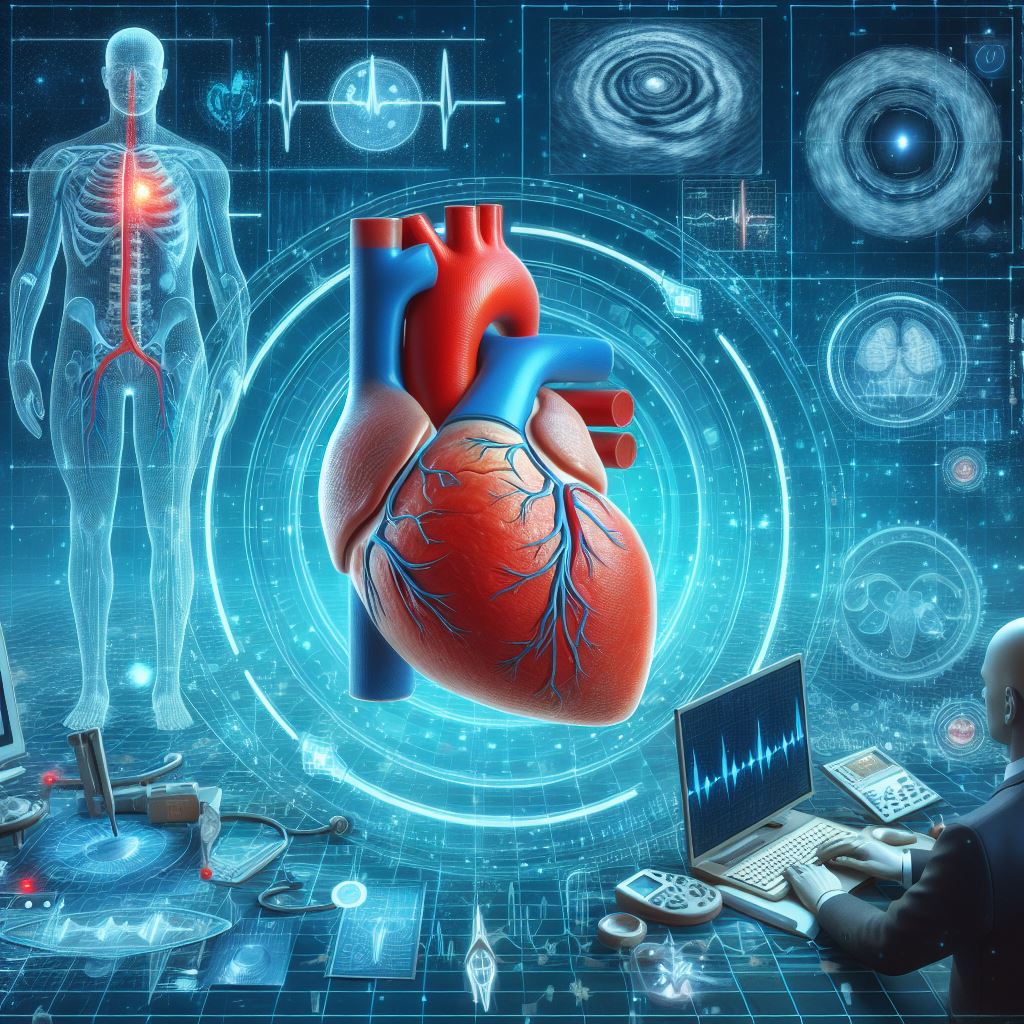
Diagnosis
·
In the realm of
cardiovascular health, timely and accurate diagnosis is the linchpin for
effective management of conditions such as blood clots. Cardiology, we employ a
comprehensive approach to diagnosing blood clots, utilizing state-of-the-art
techniques and a wealth of experience to provide our patients with the highest
standard of care.
·
Ultrasound Imaging:
A cornerstone in the diagnosis of blood clots is the use of ultrasound imaging.
This non-invasive technique allows for the visualization of blood flow and the
identification of clots within veins. By capturing real-time images, ultrasound
provides a dynamic view of the circulatory system, enabling our skilled
technicians to pinpoint the location and size of potential blood clots.
·
D-dimer Test:
The D-dimer test is a valuable tool to assess the presence of blood clots. When
a blood clot dissolves, it releases a substance called D-dimer into the
bloodstream. Elevated levels of D-dimer may indicate the ongoing breakdown of
clots within the body. While this test is sensitive, it is not specific to
blood clots and can be influenced by other conditions. As such carefully
interprets the results in conjunction with clinical findings.
·
CT or MRI Scans:
For a more detailed and comprehensive evaluation, Dr. may recommend
computed tomography (CT) or magnetic resonance imaging (MRI) scans. These
imaging modalities provide high-resolution images of blood vessels, offering a
detailed view of potential clots and their impact on circulation. CT pulmonary
angiography is particularly effective in detecting pulmonary embolisms, a
serious consequence of blood clots migrating to the lungs.
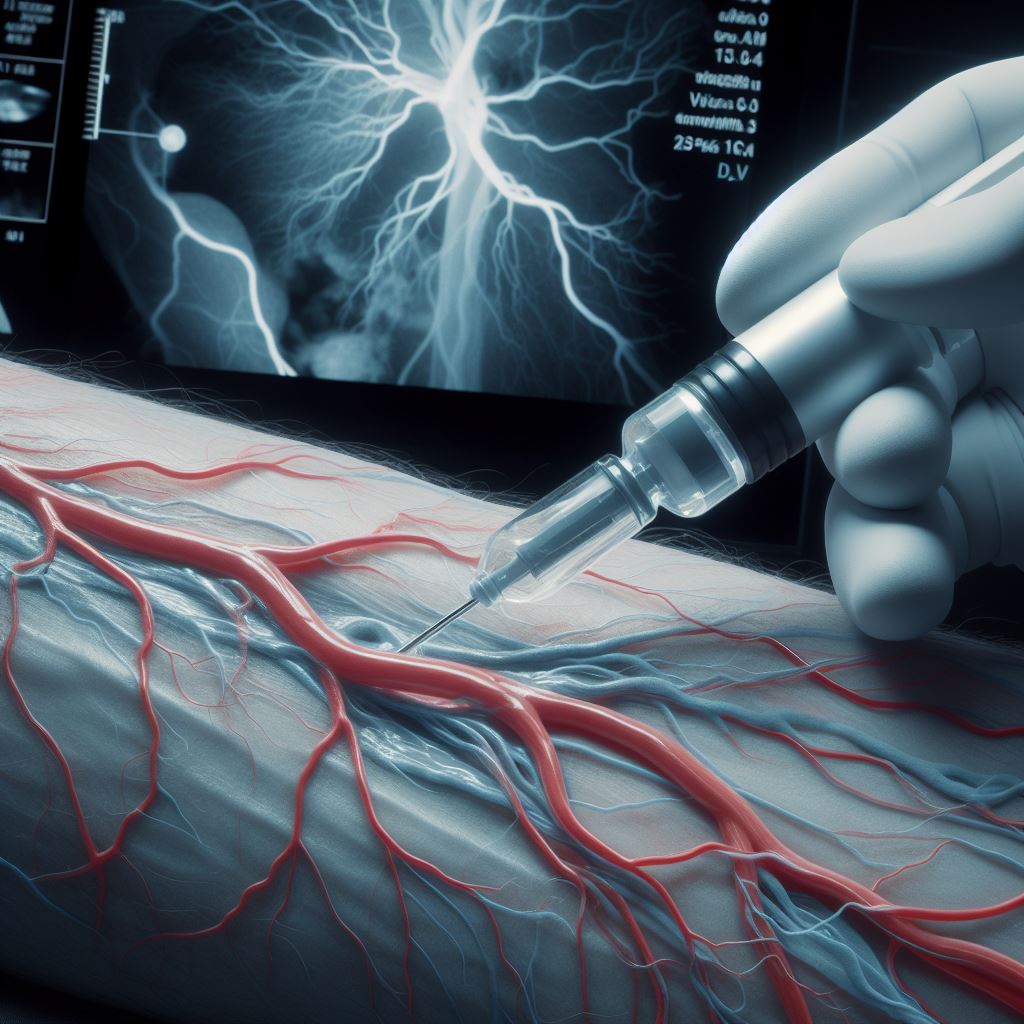
·
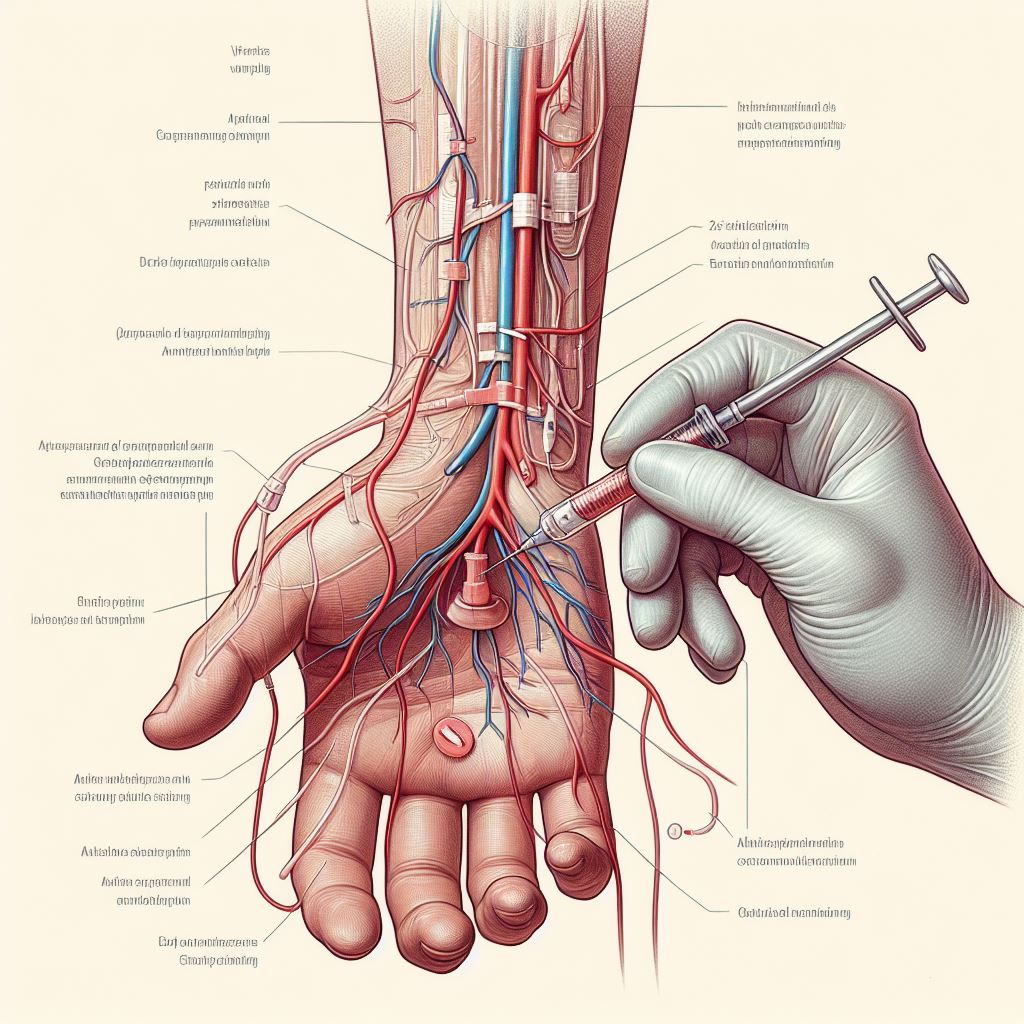
Venography:
In certain cases, venography may be employed to visualize the veins directly.
This procedure involves injecting a contrast dye into a large vein, typically
in the foot or ankle, and taking X-ray images. Venography provides a clear
picture of the venous system and can help identify blockages caused by blood
clots.
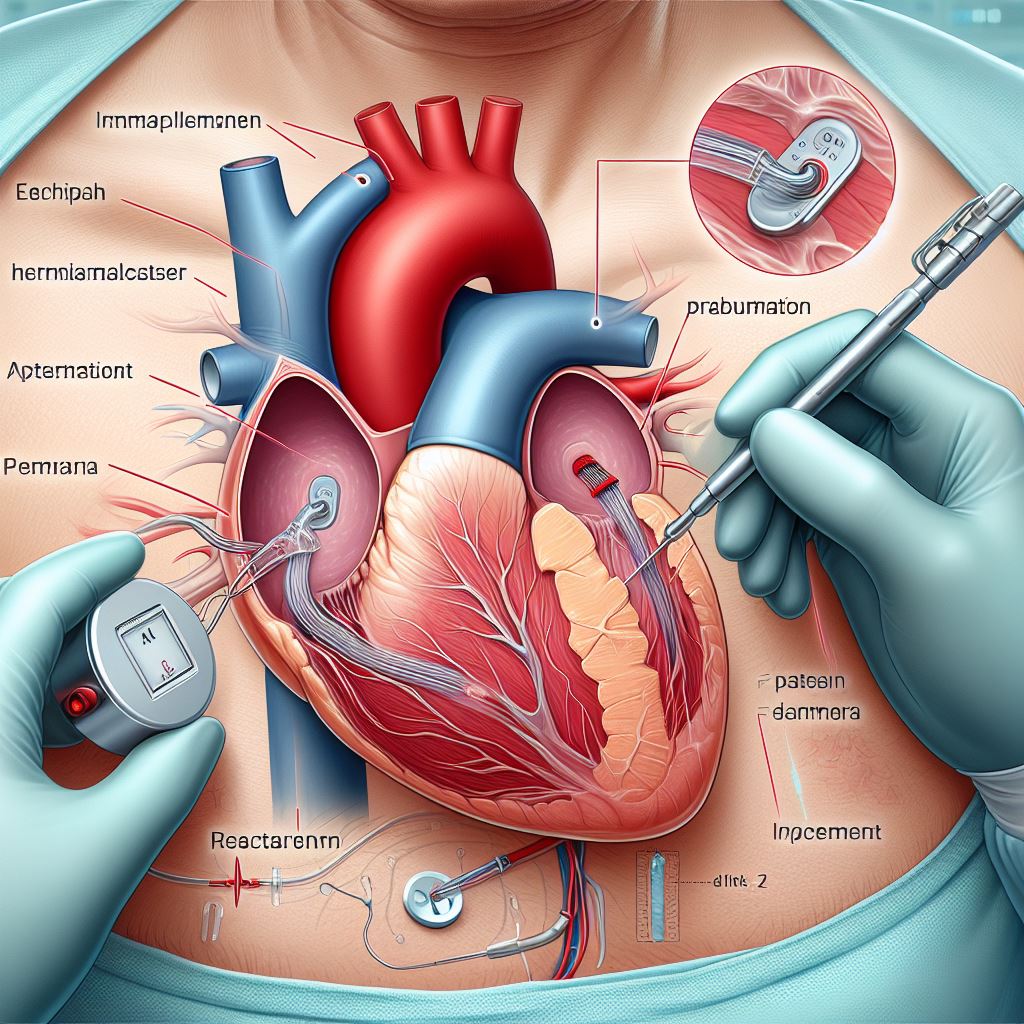
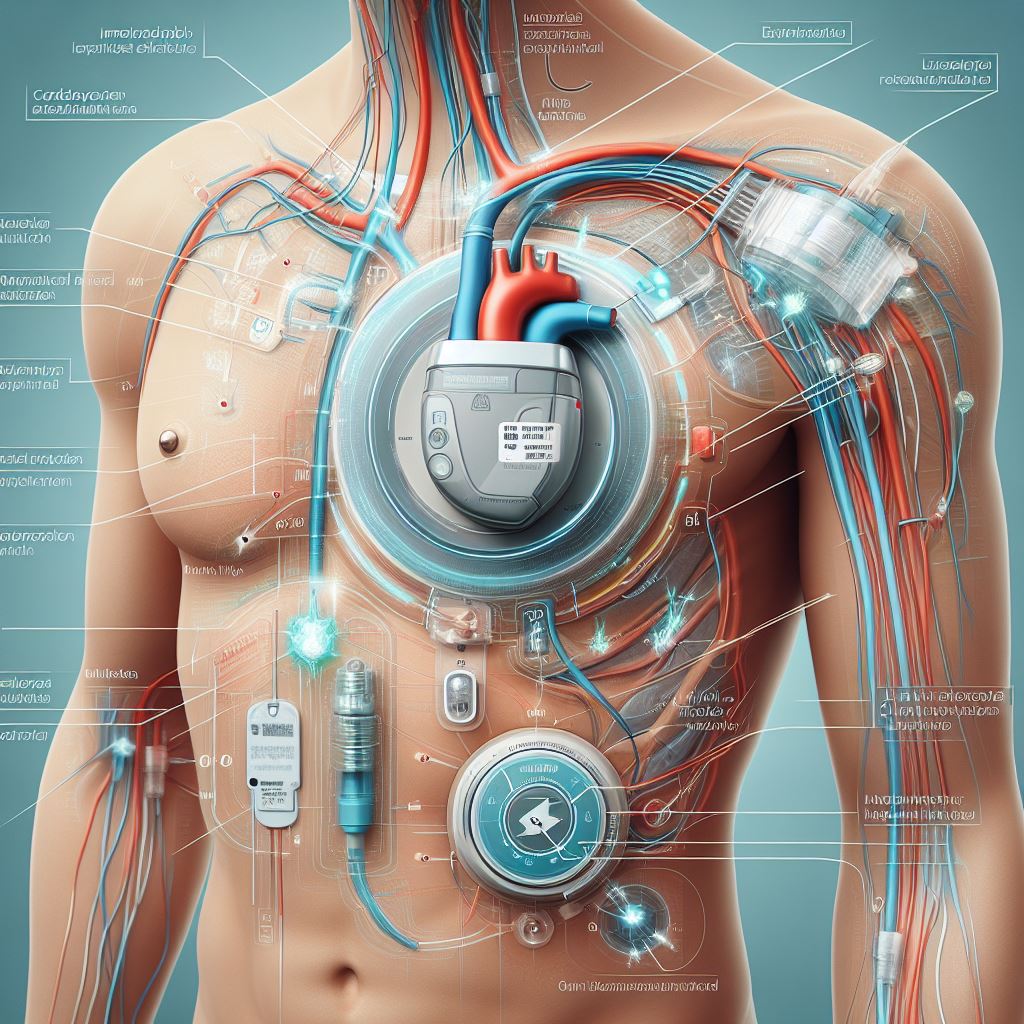
Treatment Approaches
·
At the forefront of
cardiovascular care lies the commitment to providing personalized and effective
treatment strategies for conditions like blood clots. When it comes to managing
blood clotting disorders, a multifaceted approach is essential. Below, we
explore various treatment modalities that may be recommended based on the
nature, location, and severity of blood clots, fostering a comprehensive
understanding of the options available to patients.
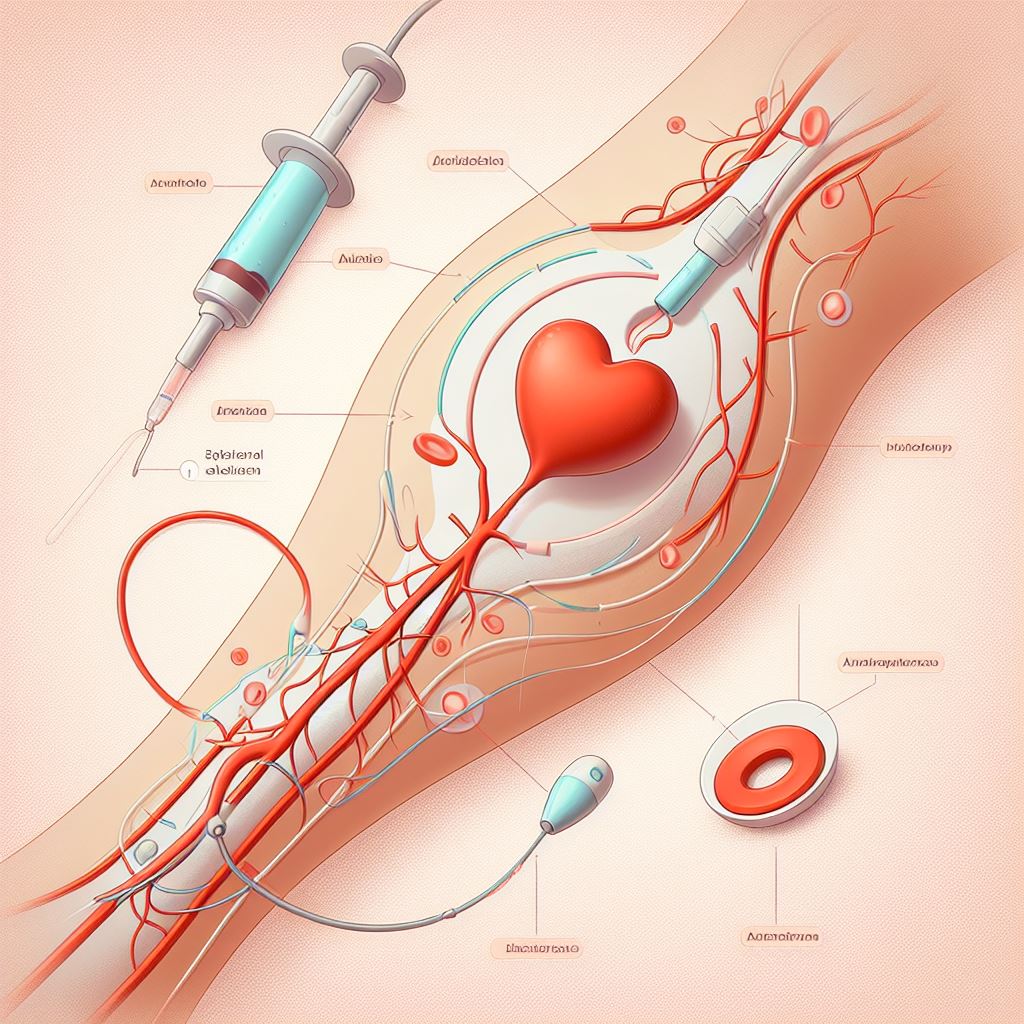
·
Anticoagulant
Medications: A primary line of defense against blood
clots involves the use of anticoagulant medications. These medications,
commonly known as blood thinners, work by inhibiting the body's clotting
mechanisms, reducing the risk of excessive clot formation. Warfarin and heparin
are examples of anticoagulants that are often prescribed. Close monitoring and
periodic adjustments are crucial to maintain the delicate balance between
preventing clots and avoiding excessive bleeding.
·
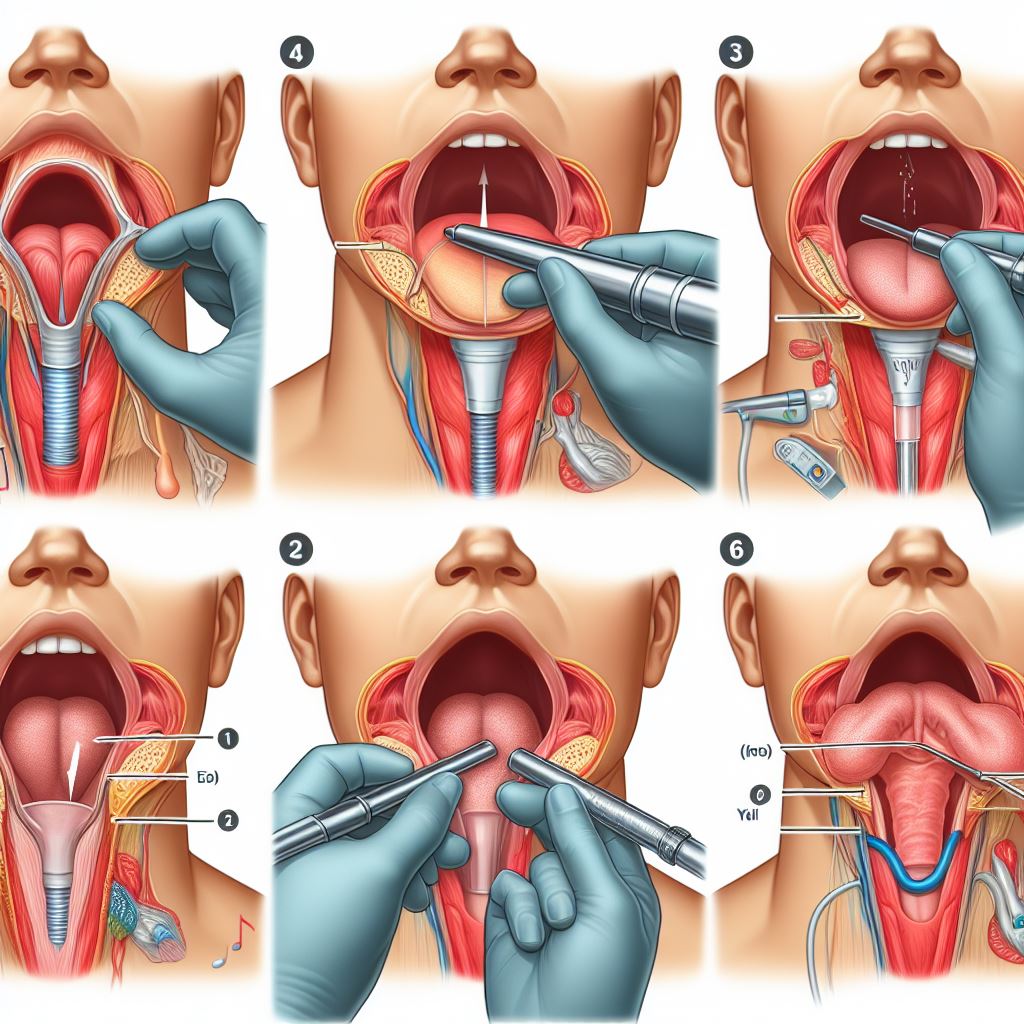
Thrombolytic Therapy:
In situations where a rapid dissolution of blood clots is imperative,
thrombolytic therapy may be employed. This treatment involves the
administration of medications, such as tissue plasminogen activators (tPAs),
that actively break down clots. Thrombolytic therapy is often reserved for
emergencies, such as acute pulmonary embolisms or severe arterial clots.
·
Vena Cava Filters:
For individuals at risk of recurrent pulmonary embolisms or those unable to
tolerate anticoagulant therapy, the insertion of a vena cava filter may be
considered. This small device is placed in the vena cava, the large vein that
carries deoxygenated blood to the heart, to trap and prevent clots from
reaching the lungs. While effective, vena cava filters are typically considered
when other treatment options are unsuitable.
·
Compression Stockings:
Especially beneficial for individuals with a history of deep vein thrombosis
(DVT), compression stockings exert pressure on the legs, promoting blood flow
and reducing the risk of clot formation. These stockings are designed to
alleviate symptoms such as swelling and pain, playing a preventive role in
managing blood clotting disorders.
·
Lifestyle Modifications:
Lifestyle plays a pivotal role in managing and preventing blood clots. Regular
exercise, maintaining a healthy weight, and avoiding prolonged periods of
immobility are essential components of a heart-healthy lifestyle.
Prevention Strategies
Preventing
blood clots is a collaborative effort that combines patient engagement and
informed lifestyle choices. At the core of cardiovascular health is a
commitment to proactive measures that reduce the risk of blood clot formation.
Here, we explore a range of preventive strategies that individuals can adopt to
safeguard their cardiovascular well-being.
·
Lifestyle Modifications:
Adopting a heart-healthy lifestyle is a cornerstone of blood clot prevention.
Regular physical activity not only promotes overall cardiovascular health but
also encourages proper blood circulation, reducing the likelihood of clot
formation. Engaging in activities such as walking, swimming, or cycling can
contribute significantly to maintaining optimal blood flow.
·
Balanced Diet:
Nutrition plays a pivotal role in preventing blood clots. A diet rich in
fruits, vegetables, and whole grains provides essential nutrients and fiber
that support heart health. Omega-3 fatty acids found in fish, flaxseeds, and
walnuts are known for their anti-inflammatory properties, contributing to a
healthier cardiovascular system.
·
Hydration:
Staying adequately hydrated is crucial for maintaining blood viscosity. Proper
hydration helps prevent the blood from thickening, reducing the risk of clot
formation. Individuals should strive to drink an ample amount of water
throughout the day, particularly in situations that may lead to dehydration.
·
Smoking Cessation:
Smoking is a significant risk factor for blood clots. The chemicals in tobacco
can damage blood vessels and increase the likelihood of clot formation.
Quitting smoking is one of the most impactful steps individuals can take to
enhance their cardiovascular health and reduce the risk of blood clots.
·
Medication Management:
For individuals with underlying medical conditions or risk factors for blood
clots, adherence to prescribed medications is essential. Anticoagulant
medications, when prescribed, should be taken as directed to maintain their
effectiveness in preventing clot formation.
·
Compression Stockings:
Particularly beneficial for those at risk of deep vein thrombosis (DVT),
compression stockings exert pressure on the legs, promoting healthy blood flow.
Individuals who spend prolonged periods sitting or standing, such as during
long flights, can benefit from the use of compression stockings to reduce the
risk of clot formation.
·
Regular Check-ups:
Routine medical check-ups are integral to proactive healthcare. Regular visits
to healthcare providers allow for the monitoring of cardiovascular health and
the identification of potential risk factors for blood clots. Open
communication with healthcare professionals enables early intervention and the
implementation of preventive measures.